The Ontario Health Study Newsletter, November 2019
Nov 1, 2019 // OHS Newsletter

In this Issue:
- The OHS Work History Questionnaire closes December 1st
- Top 6 reasons this epidemiologist is interested in your work history
- Precision medicine will lead to precision policy
- New collaboration streamlines cancer research data projects
- Halifax researcher eyes Ontario data for future study
- New team member takes the lead on OHS biosamples
- Why did you do the Work History Questionnaire?
The OHS Work History Questionnaire closes December 1st
Only a few weeks remain to complete your OHS Work History Questionnaire! Over 22,000 OHS participants have already told us their work story, and you have until December 1st, 2019 to tell us yours.
We spend a lot of our time at work – it makes up a significant portion of our lives and can influence our health in many ways that are being investigated by scientists and health researchers.
Even if you cannot complete the entire questionnaire in one sitting, or you’ve have had more jobs than you can remember, every bit of information you provide is of great importance to researchers. Similarly, if you are retired or not currently working, the information you provide is also extremely valuable. Some diseases and conditions can take a long time to develop, so a job you had many years ago may still play a role in your current health.
Your work stories are crucial to understanding the many ways our work can have an impact on our health, such as the type of job, hours of work, your commute, chemical exposures, stressful work environments and much more.
You can do it! Click here to log into your account and complete the Work History Questionnaire by December 1st.
Top 6 reasons this epidemiologist is interested in your work history

Why is it so important to study occupational exposures? We asked epidemiologist Vikki Ho, research scientist with University of Montreal Hospital Research Centre (CRCHUM), who has applied to use OHS questionnaire data for her research into the occupational risks of exposure to a wide range of chemicals.
- The work environment makes for rich research. Although most chemicals and other agents found in the workplace are also found in the general and home environment, workers tend to be exposed to things at higher concentrations, more frequently, and for longer durations. So it’s ideal to study the occupational environment, according to Dr. Ho, who is also an assistant professor in the School of Public Health at the University of Montreal. The health effects of these exposures can have an impact on the rest of your life.
- Your occupational history is just as important as your health history. “If I only know how much you sleep, how much you eat, or if you run in the afternoon, I don’t know what you’re doing the rest of the time. And I would say those work exposures do matter a great deal,” said Dr. Ho. “The OHS Work History Questionnaire would give us a cumulative look at everything you’ve been exposed to over your lifetime so that we can evaluate the impact of these exposures on long- and short- term health.”
- Older workers’ exposures to chemicals or environments allow a valuable moment-in-time comparison. A dry-cleaner working in the 1960s would have been exposed to benzene, a chemical banned in the 1970s. A dry-cleaner working in the 2000s will have been exposed to its ‘safer’ derivatives, Toluene and Xylene. “We need period-specific data to assess different exposures and risk levels over time.”
- Sometimes we don’t know what we don’t know yet. That’s where population-based studies like the OHS can prove valuable in providing the evidence to move to better health policy. “Sometimes we use a chemical on the job up until we know it’s harmful, or we use a chemical at low doses and only later find out it's harmful to be exposed to it over a long period of time,” she said. “Policy does aim to prevent hazardous workplaces, but we can’t always have the full picture when we need to make a decision about ‘where do we set the limit now’.”
- More data about occupational risk is better data. Ho noted there are many research initiatives in her specialty area of occupational exposures and cancer. However, in order to build a case that a substance is highly likely to be carcinogenic, it is important that the same results be obtained from multiple studies, looking at many different groups of people. Only then can we move towards good public health policy and regulation.
Her work tends to focus on people who already have a cancer diagnosis. “But as good a job as I can do to minimize all the errors with estimated exposure, there’s still inherently the possibility of error of everyone having to think back in time,” she said. “That’s why we need lots of different types of studies – like the OHS, which is collecting information before people are diagnosed with certain diseases – to understand exposure before disease onset.”
- When we can replicate findings, that’s when it can fuel policy change. Leaded gas was available in Canada as late as 1990. Workers could smoke at their desks until the mid-1990s. Asbestos was used as a home insulation material from the 1930s to the 1990s. It was evidence-based research that eventually lead to governments banning such practices. “Right now there are initiatives like the OHS, taking place in many countries. And if everyone finds the same results, it can definitely lead to health policy changes.”
Click here to log into your account and complete the Work History Questionnaire by December 1st.
Precision medicine will lead to precision policy
Discoveries from the Canadian Partnership for Tomorrow Project (CPTP), Canada’s largest health data collection project, point to huge potential for precision medicine to be used with targeted health policies.
New evidence could help Canadian scientists and policy-makers transform how chronic diseases are treated. For example, a study last spring led by OHS Executive Scientific Director Dr. Philip Awadalla and a team of Canadian researchers found strong evidence that environmental exposure has a significantly stronger impact than ancestry on the regulation of genes and their impact on disease.
The discovery came out of one of the largest studies yet to examine the relationship between genetics and environmental stimuli, and the data paves the way for precision medicine and targeted policies to be used together to support healthy living.
Read Dr. Awadalla’s op-ed published in Policy Options, a digital magazine for Canadian policy-makers.
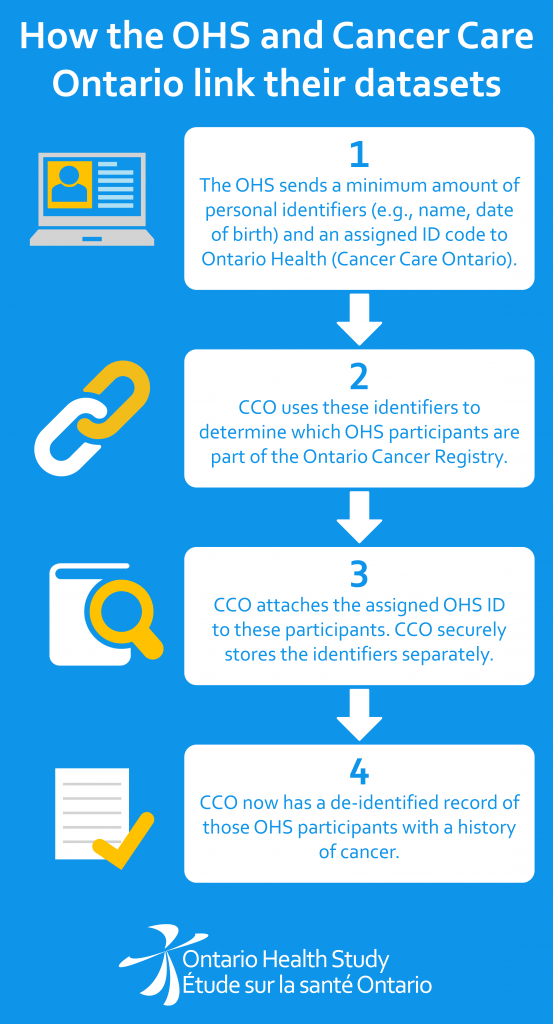
New collaboration streamlines cancer research data projects
The OHS has just made it faster for researchers to access Ontario’s cancer records and link them up with the health questionnaire information and blood samples already provided by Study participants.
Two years ago, Dr. Philip Awadalla began a research question that asked: What if we could identify ‘markers’ in a person’s genes or blood that could foreshadow the presence of a cancer, years ahead of an actual diagnosis?
Dr. Awadalla applied to the OHS for permission* to draw data about a pool of OHS participants, for whom there was a blood sample as well as questionnaire data about self-reported health and lifestyle information. To get cancer records of the OHS participants, Dr. Awadalla also had to make a separate, parallel request to access the Ontario Cancer Registry.
This step would have needed to be repeated by every other scientist asking to look at OHS data about participants who reported having cancer. For each request, the keeper of the Ontario Cancer Registry, Cancer Care Ontario (CCO), would need to create a new, separate cancer data set.
Fast forward to this summer, when the OHS completed an important data linkage initiative involving the entire OHS data set and the Ontario Cancer Registry record holdings. This was only possible because 96% of OHS participants have agreed to allow OHS to link to their administrative health data such as OHIP records and the Ontario Cancer Registry. (Learn more about how administrative health data works in this short video from Population Data BC.)
The new OHS agreement means Cancer Care Ontario now holds a ready-made, stand-alone data set containing records of only OHS participants who have a medical record relating to cancer after enrolling in the Study. Because that data set remains securely held inside CCO, and is updated annually, the privacy of Study participants is safeguarded.
It also means that four other researchers currently pursuing OHS cancer-related research projects, and all those who come after them, will get their OHS cancer data sets much more quickly.
 |
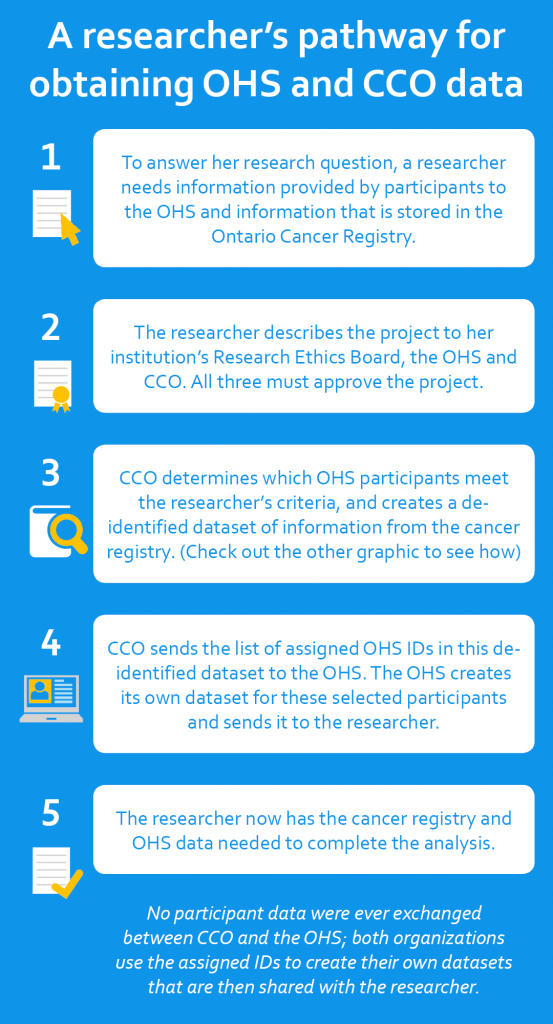 |
“We now have a fast-track process to get data into the hands of researchers without having to re-create the linkage for every single project,” said Dr. Awadalla. “This saves time and resources for the researcher, Cancer Care Ontario and OHS. Without this collaboration, many of the same steps would have had to be repeated every time a new project was approved.”
While 20,857 of our 225,000 participants told OHS they experienced a cancer diagnosis, the Ontario Cancer Registry holds much more detailed information about how each cancer is diagnosed, the stage of diagnosis, and any subsequent cancer treatments.
*Though Dr. Awadalla is the Executive Scientific Director of the Ontario Health Study, and an active researcher in his own right, he nevertheless had to apply to have his research project reviewed and approved by the OHS Data Access Committee.
Halifax researcher eyes Ontario data for future study

A Halifax researcher is already interested in seeing how the Work History questionnaire data from Ontario participants will stack up against those from Atlantic Canada.
Dr. Ellen Sweeney is the Director of Strategic Research Initiatives for Atlantic PATH, a sister study to the OHS. Similar to what the OHS is now doing, Atlantic PATH asked its 30,000 participants questions about their past jobs and occupational exposures as part of its baseline data collection (2009-2015).
Dr. Sweeney and her team recently published their first findings from that investigation. It found an association between shiftwork and a higher risk of cardiovascular disease, obesity and diabetes. “Even though these people who did shiftwork had higher levels of physical activity and lower levels of sedentary behavior – which is what we all tell people they should do – they still had these health issues. So, there’s more going on here.”
Dr. Sweeney is watching the current OHS Work History Questionnaire with interest. She said it would be very interesting to compare the data from the Atlantic PATH study with those of the OHS. “If there are similarities between our findings and the OHS, that strengthens the work overall. If there are differences, it’s important to look at them and see if there are other variables at play, either here or in Ontario, that are influencing the health of participants,” she said from Halifax.
She hopes OHS participants will recognize the value of sharing the history of the jobs they’ve held over the years.
“Yes, it can be somewhat onerous for the participant in terms of the figuring out ‘how much time do I spend sitting every day?’ or ‘what was my job 30 years ago?’ But this data will give us insight into health research in a way that supplements the questionnaires they’ve already completed,” she said.
“If you’ve only filled out the health questions, we don’t have data about your occupation, and we don’t have information that could tell us whether your work is influencing your health and if there’s an association between the two. There are still things to learn that we can’t learn without this information.”
Here’s the type of research your OHS questionnaire could generate!
Why is your work history important to us? Because it is a key part of your health history. This research paper, from our sister study, Atlantic PATH, showed a link between shift work and an increased risk of heart disease, obesity and diabetes in Atlantic Canadians – even though the workers were more physically active.
Click here to log into your account and complete the Work History Questionnaire by December 1st.
New team member takes the lead on OHS biosamples
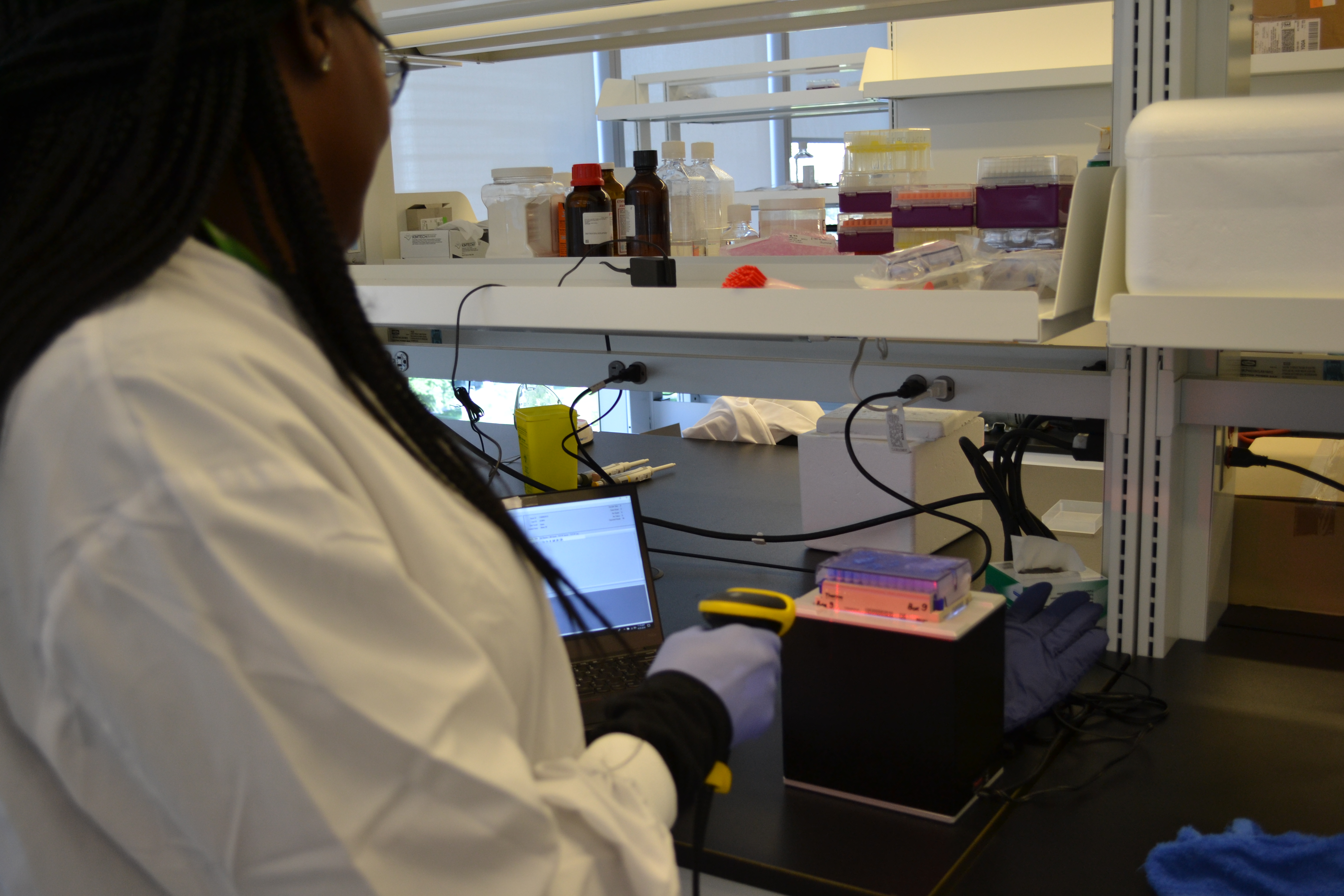
This summer Abiola Oduwole joined the OHS as Project Lead, Biospecimen Operations to organize, manage and process the many thousands of biosamples so generously provided by our participants and prepare them for use by approved researchers. Here she is barcoding and scanning DNA samples extracted from blood, to confidentially catalog which participant it is linked to, and where each sample is securely stored.
Welcome to the team, Abi!
Why did you do the Work History Questionnaire?

Here’s what Hilary from Chatham had to say:
“Why did I take the work questionnaire? Really I did it because I love questionnaires and the thought of being a statistic. I am fascinated by the possibilities of the OHS and feel proud to be a part of it. Answering the work questionnaires was a wonderful trip down memory lane.”
We love hearing from you. As an OHS participant, why will you take the Work History questionnaire? Email us at info@ontariohealthstudy.ca
Click here to log into your account and complete the Work History Questionnaire by December 1st.